Our health care system has been built up over the years in a jury-rigged, ramshackle fashion. Before World War II, there was very little health insurance and what there was often was the product of labor union contracts. The early years were concerned with accident insurance and workers compensation laws.
The American life insurance system was established in the mid-1700s. The earliest forms of health insurance, how ever, did not emerge until 1850, when the Franklin Health Assurance Com pany of Massachusetts began providing accident insurance, to cover injuries re lated to railroad and steamboat travel. From this, sickness insurance covering all kinds of illnesses and injuries soon evolved, but the first modern health insurance plans were not formed until 1930.
The Baylor program for school teachers was the first in 1929.
Medical insurance took stride in 1929 when Dr. Justin Ford Kimball, an administrator at Baylor University Hospital in Dallas, Texas, realized that many schoolteachers were not paying their medical bills. In response to this problem, he developed the Baylor Plan teachers were to pay 50 cents per month in exchange for the guarantee that they could receive medical services for up to 21 days of any one year.
In those days, the concern was lost wages more than hospital care.
In 1939, the American Hospital Association (AHA) first used the name Blue Cross to des ignate health care plans that met their standards. These plans merged to form Blue Cross under the AHA in 1960. Considered nonprofit organizations, the Blue Cross plans were exempted from paying taxes, enabling them to maintain low premiums. Pre-paid plans covering physician and surgeon services, includ ing the California Physicians’ Service in 1939, also emerged around this time. These physician-sponsored plans com bined into Blue Shield in 1946 and Blue Cross and Blue Shield merged into one company in 1971.
The modern insurance plans were very recent in origin. I was there for much of it. The commercial insurers fought the status of Blue Cross, which was not required to have reserves. Blue Cross asserted that it promised hospital care, not payment, so reserves were not necessary.
The 1940s and 1950s also saw the proliferation of employee benefit plans, and the included health insurance pack ages became more and more compre hensive as strong unions negotiated for additional benefits. During the Second World War, companies competing for labor had limited ability to use wages to attract employees due to wartime wage controls, so they began to compete through health insurance packages. The companies’ healthcare expenses were exempted from income tax, and the resulting trend is largely responsible for the workplace’s present role as the main supplier of health insurance.
The war produced much of this as wage limitations were in force but fringe benefits, like health insurance, were permitted. A lot of this history is contained in Paul Starr’s book The Social Transformation of American Medicine.
From the first, commercial insurers focused on employer plans while Blue Cross and Blue Shield (which was founded by the California Medical Association to pay doctor bills) were individual plans.
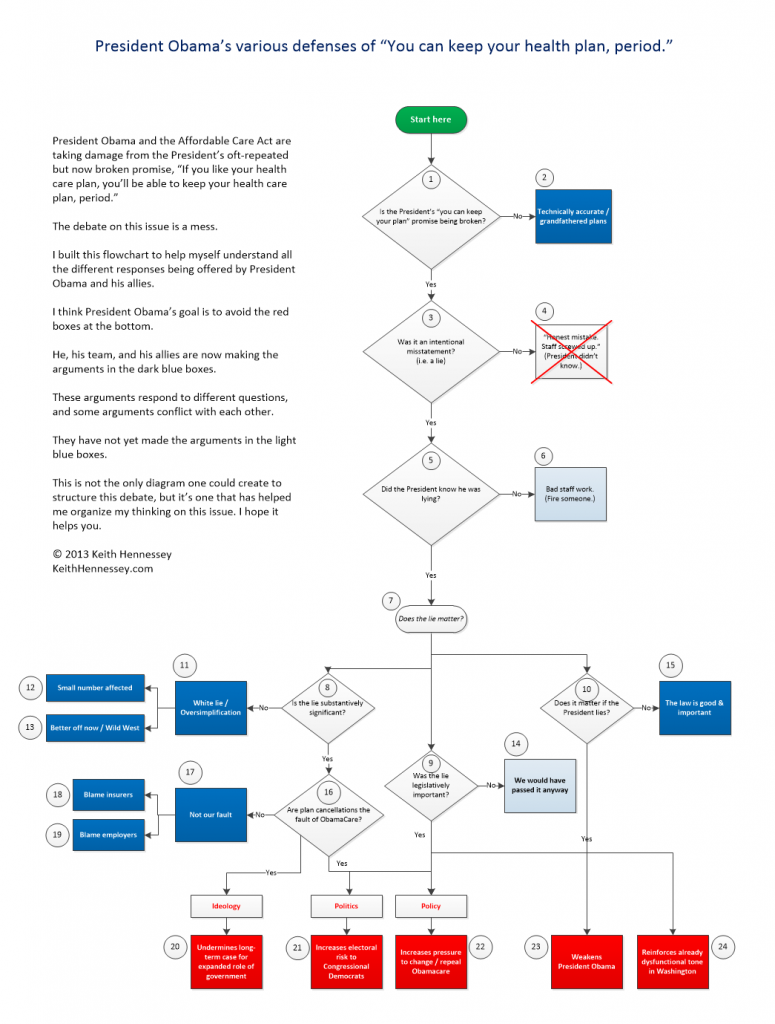
In 1954, Social Security coverage included disability benefits for the first time, and in 1965, Medicare and Medicaid pro grams were introduced, in part because of the Democratic majority in Congress. In the 1970s and 1980s, more expen sive medical technology and flaws in the health care system led to higher costs for health insurance companies. Responding to higher costs, employee benefit plans changed into managed care plans, and Health Maintenance Organizations (HMOs) emerged. Man aged care plans are unique in that they involve a particular network of health care providers that have been verified for healthcare quality and that have agreements with the insurer about price and related issues. HMOs were originally primarily nonprofit, but they were quickly replaced by commercial interests, and managed care only suc ceeded in temporarily slowing the growth of healthcare costs.
Two major changes came in the 1970s. In 1978, the federal government established what were called Professional Standards Review Organizations or PSRO. All doctors had to receive training in how to do these reviews and it was immediately apparent that cost was the only consideration, not quality of care.
I decided to educate myself and took a course from an organization called “The American Board of Quality Assurance and Utilization Review Physicians. I took the exam and passed, then attended the annual meeting. This was about 1986. People I met at that meeting informed me that the exams were graded by throwing them up in the air. Any that landed balancing on one edge were flunked. Nonetheless, the experience was valuable because I could see what was coming.
I was president of the Orange County Medical Association that year and had served for eight years on the Commission on Legislation of the CMA, now called The Council on Legislation. This gave me an opportunity to meet many legislators, many state level and some federal. The impression they made on me was that few knew anything about medicine and most were not very intelligent.